Over the last few years there has been an increase in self-harm by children and adolescents in England, rates have been found to increase rapidly, especially during adolescence (Morgan et al., 2017). With there being greater awareness of self-harm through mental health campaigns and media attention including coverage on the news and drama series, is the reporting of self-harm improving due to better awareness, or are young people really self-harming at increasing rates? How concerned should we be about the increase? In this blog, I draw on recent work by my colleagues in the Multicentre Study of Self-Harm in England.

The Multicentre Study of Self-Harm in England
The Multicentre Study is a three-site collaboration between the University of Manchester, the University of Oxford and Derbyshire Healthcare NHS Foundation Trust. It involves the collection of detailed data on self-harm from hospital emergency department presentations across five general hospitals; three in Manchester, one in Oxford and one in Derby. As a result, this longitudinal study has over 15 years (and counting!) of data on demographics of individuals that have self-harmed, detailed methods of self-harm, precipitants for the self-harm, clinical characteristics (psychiatric treatment, previous self-harm) and referrals from the hospital. This means we can explore trends of self-harm in different groups of individuals over-time, as well as outcomes such as repetition of self-harm.
We define self-harm as any act of intentional self-poisoning or self-injury irrespective of motivation or intent. This is the most commonly used definition in UK and European research where suicidal behavior is seen as a spectrum of behaviours (Kapur et al., 2013).
Challenges of monitoring self-harm
One of the many challenges of accurately monitoring self-harm in children and adolescents is that it can often be a hidden behaviour, many do not come to the attention of services. If they are self-harming in private and keep it hidden from parents and teachers we will not know about the extent of the problem in this group.
For those that do come to the attention of services, either through primary care such as their GP or secondary care such as presenting to the hospital emergency department for either medical treatment as a result of the self-harm or for mental health care, monitoring self-harm in these groups in essential. This also presents as an opportunity for intervention, either for the self-harm or other issues the young person is experiencing such as bullying or substance misuse, and for the identification and treatment of any underlying mental health problems.
Recent work on incidence and trends in self-harm in children and adolescents
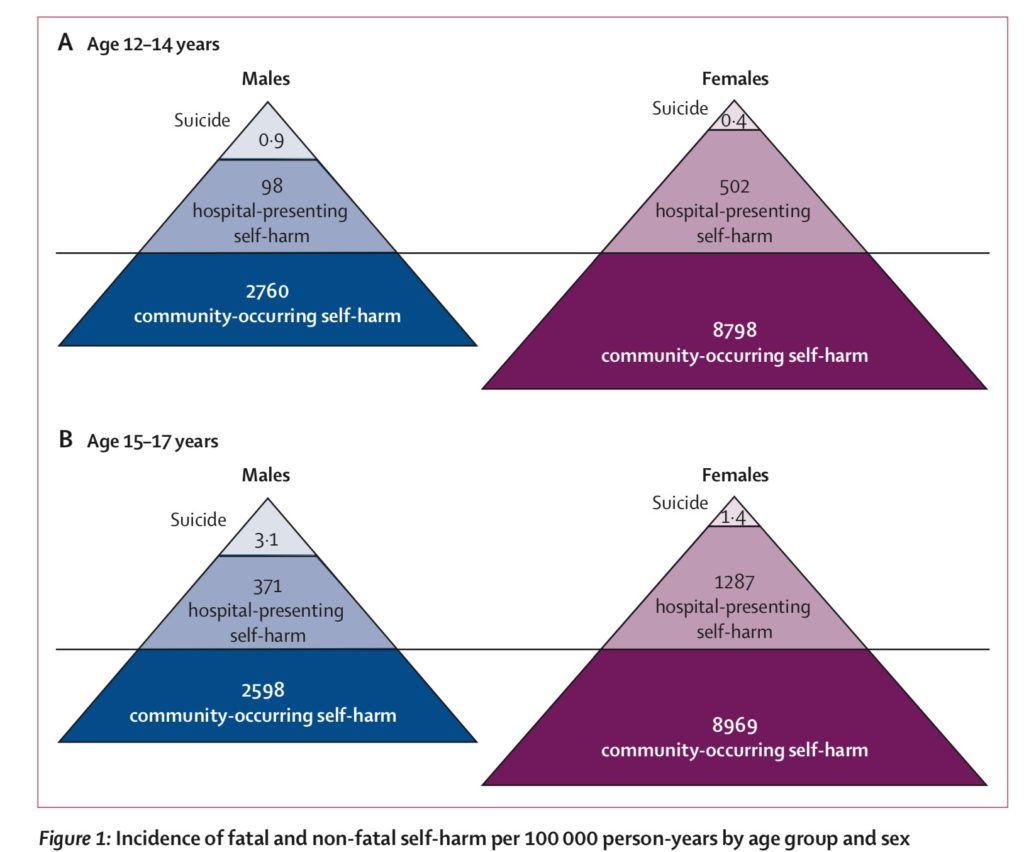
Our most recent work compared incidence of hospital-presenting self-harm, community-occurring self-harm, and suicide (Geulayov et al., 2018). Mortality (via ONS data linkage), hospital monitoring and school survey data were analysed, adolescents included in the research were aged 12-17 from England. Findings were presented in terms of an ice berg model (Geulayov et al., 2018).
Self-harm in the community/primary care
Represented by the first and largest level in the Iceberg representation, the incidence of self-harm is highest in the community. What is most concerning about this level is that it is submerged, under water, using the iceberg metaphor. Many of these children and adolescents may not even come to the attention of clinical services –it is hidden. Epidemiologically ascertained incidence rates have indicated a large-scale problem.
One study by our colleagues that made headlines in the UK was based on research on self-harm by children and adolescents aged 10-19 in primary care. Morgan et al (2017) examined incidence of self-harm using data from UK Clinical Practice Research Datalink. Findings showed incidence of self-harm in girls was higher across all age groups; more notably, the researchers found a sharp 68% increase in incidence of self-harm among young girls aged 13-16 between 2011 and 2014. Could the increase be due to greater awareness and help-seeking?
Reasons for the rise in self-harm were not explored, however it is possible that young girls tend to seek help more than boys –which could explain why the increase was not apparent in boys of the same age. However, the increase could also be a true rise in self-harm as the researchers suggest.
Nonetheless, whilst there is an urgent need for intervention for girls, especially during the ages of 13-16 in secondary schools, further research is also needed to examine what is going on in the lives of these young girls that is causing them to self-harm at increasing rates?
There is also a gap in current provision, easily accessible support for children and adolescents to intervene at an early stage is needed, especially for those that may not engage with services or those that do not meet the requirements of secondary mental health services.
One study by our research group investigated repetition of self-harm in children and adolescents, 5,205 young people aged 10-18 presented to hospital with a total of 6,598 episodes of self-harm (Hawton et al., 2012). Follow-up showed approximately 27% repeated self-harm, repetition was associated with older age, self-cutting and a previous history of self-harm and psychiatric treatment. Self-cutting was also found to be associated with increased suicide risk compared to self-poisoning by drugs.
These findings highlight that children and adolescents using self-cutting as a method of self-harm should be taken seriously, and that self-harm is not just ‘attention seeking behaviour’.
In our recent work, self-cutting was found to be the primary method of self-harm in the community. We know from previous research that self-cutting carries a greater risk of suicide. Further work is needed in understanding how and why cutting is associated with an increased risk. Qualitative work may also help understand why children and adolescent cut.
For those that do come to the attention of their GPs in primary care, further probe into reasons for self-harm and additional support is essential. It is important to note that self-harm is often a symptom of distress, rather than a treatable disorder on its’ own, therefore identifying the primary causes of self-harm behaviours should be a priority.
Although we would all like for the self-harm to stop immediately or completely, this is not always realistic. It may take time, as it has been used as a coping mechanism, particularly for those that have been self-harming for a long time to manage distress.
School-based programmes also have a role. Training for schools on responding to self-harm is important to aid prevention and reduction of risk. We know from more recent work that suicidal behaviour can occur in clusters (Hawton et al., 2019). The new guidance on identifying and responding to suicide clusters from Public Health England (2019) suggests one of the key components to a suicide cluster response is ongoing surveillance. Therefore monitoring the occurrence of any form of self-harm/suicidal act in schools and in the community should be routine practice. Young people are particularly vulnerable to ‘contagion’ effects.
School staff should also be alert to any factors contributing to the self-harm, such as bullying or harmful social media use (PHE, 2019). The guidance highlights that suicide clusters may be associated with increase in self-harm. Although monitoring self-harm in the community is difficult, one approach is to monitor self-harm that results in an emergency department hospital presentation. This is important to detect trends in specific ages.
Emergency Department hospital presentations for self-harm
The second level of the ‘iceberg’ in the model represents hospital-presenting self-harm. These children and adolescents do come to the attention of clinical services. One key finding at this level was the significant difference in incidence of self-harm between the younger and older adolescents. This difference was not evident in the community sample. Girls aged 15-17 had the highest incidence of both hospital-presenting and community-occurring self-harm.
This level of the iceberg is the perfect opportunity for intervention. It is therefore vital that hospital-based services are well resourced and a thorough psychosocial assessment is provided to all children and adolescents. Previous research has found psychosocial assessments to be beneficial and reduce risk of self-harm repetition (Carroll et al., 2016; Steeg et al., 2018). Appropriate aftercare arrangements are also important at this level, including psychological treatment if necessary or signposting/ referral to third sector services. It is equally important that community mental health services are easily accessible for these young people as it shows they are willing to seek help.
Our research suggests that those who repeat self-harm, repeat quickly (Kapur et al., 2006). Therefore early follow-up care is essential.
The NICE guidelines on the management of self-harm recommend that:
- All children and adolescents should be admitted overnight to a paediatric ward and assessed fully prior to discharge.
- They should have access to CAMHS and substance misuse services.
- Assessment should also include a full evaluation of the family, their social situation, and child protection issues & any referrals should be based on the needs identified.
- Each repeat self-harm episode should be treated in its own right as the reasons for self-harm may be different on each occasion.
Finally, the extent of the problem for the whole of England was estimated: approximately 21,000 children and adolescents (aged 12-17) present to general hospital following self-harm; but 200,000 self-harm in the community and do not present to hospital. These stark figures emphasize the great population burden of self-harm and the scale of the problem. It is likely that reporting of self-harm is improving due to better awareness, however it is equally possible that there is an increase in self-harm, further research is needed to understand reasons for the increase.
There is a role for school-based interventions at the community level. Perhaps training in, and responding to and supporting children and adolescents that self-harm should be mandatory across all schools, just as physical first aid training is compulsory? Schools offer the unique opportunity for early intervention and identification of any emerging mental health problems.
Going back to my original question, how concerned should we be about the recent increases in self-harm? Our work brings attention to a large number of young people self-harming in the community –and not in contact with services, using cutting as a method of self-harm –which we know carries greater suicide risk. Although many that self-harm may not have suicidal intentions, intent can change over-time, and self-harm is the strongest risk factor for suicide in adolescents (Hawton et al., 2012; Kapur et al., 2013). Therefore, it should not be taken lightly. It is also possible that self-harm could be adopted as a maladaptive coping strategy, leading to repetition of this behavior -which could continue into adulthood.
The key take-home message is that self-harm should be taken seriously, and that medical severity should not be used as a marker for level of distress.
Conflicts of interest
Bushra works within the Multicentre Study for Self-Harm in England, which is funded by the UK Department of Health and Social Care. She has no financial interests in the work.
References
Carroll, R., Metcalfe, C., Steeg, S., Davies, N. M., Cooper, J., Kapur, N., & Gunnell, D. (2016). Psychosocial Assessment of Self-Harm Patients and Risk of Repeat Presentation: An Instrumental Variable Analysis Using Time of Hospital Presentation. PLOS ONE, 11(2), e0149713.
Geulayov, G., Casey, D., McDonald, K. C., Foster, P., Pritchard, K., Wells, C., Clements, C., Kapur, N., Ness, J., Waters, K., & Hawton, K. (2018). Incidence of suicide, hospital-presenting non-fatal self-harm, and community-occurring non-fatal self-harm in adolescents in England (the iceberg model of self-harm): A retrospective study. The Lancet Psychiatry, 5(2), 167–174.
Hawton, K., Bergen, H., Kapur, N., Cooper, J., Steeg, S., Ness, J., & Waters, K. (2012). Repetition of self-harm and suicide following self-harm in children and adolescents: Findings from the Multicentre Study of Self-harm in England: Repetition and suicide after self-harm. Journal of Child Psychology and Psychiatry, 53(12), 1212–1219.
Hawton, K., Hill, N. T. M., Gould, M., John, A., Lascelles, K., & Robinson, J. (2019). Clustering of suicides in children and adolescents. The Lancet Child & Adolescent Health. https://doi.org/10.1016/S2352-4642(19)30335-9
Kapur, N., Cooper, J., King-Hele, S., Webb, R., Lawlor, M., Rodway, C., & Appleby, L. (2006) The repetition of suicidal behaviour: a multicentre cohort study. The Journal of Clinical Psychiatry, 67(10), 1599-609.
Kapur, N., Cooper, J., O’Connor, R., & Hawton, K. (2013). Non-suicidal self-injury v. attempted suicide: new diagnosis or false dichotomy? The British Journal of Psychiatry, 202, 326-328.
Morgan, C., Webb, R. T., Carr, M. J., Kontopantelis, E., Green, J., Chew-Graham, C. A., … Ashcroft, D. M. (2017). Incidence, clinical management, and mortality risk following self harm among children and adolescents: Cohort study in primary care. BMJ, j4351.
NICE (2004) Self-harm in over 8s: Short-term management and prevention of recurrence. London: National Institute for Health and Care Excellence.
Public Health England. (2019). Identifying and responding to suicide clusters. Retrieved from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/839621/PHE_Suicide_Cluster_Guide.pdf
Steeg, S., Emsley, R., Carr, M., Cooper, J., & Kapur, N. (2018). Routine hospital management of self-harm and risk of further self-harm: Propensity score analysis using record-based cohort data. Psychological Medicine, 48(2), 315–326.



Discussion
Thank you for doing this important research. As a mother of an adolescent who self harms, I understand how vital research is needed into understanding the causes of self harm. Children are struggling, parents and families are struggling and the mental health services are so desperately underfunded. We want to help our children and other young people experiencing this awful situation.